Genomics
Institute

IGI Sickle Cell Initiative
The IGI is working to bring CRISPR-based sickle cell disease therapies to the world — and make them accessible
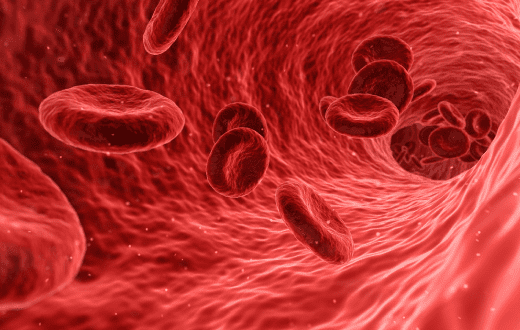
Sickle cell disease is a genetic disease that affects nearly 100,000 Americans and millions more globally, disproportionately affecting people of African descent. People with sickle cell disease share a single-letter DNA mutation that causes red blood cells to become crescent-shaped, or "sickled." These distorted cells can block blood vessels, causing immense pain and poor oxygen transport through the body. In addition to chronic pain, complications include organ damage, strokes, and anemia, and it can be fatal.
At the IGI, we are developing new CRISPR-based treatments and companion diagnostics for sickle cell disease, and ways to make it affordable.
Treating Sickle Cell Disease

The IGI vision is to develop a cure for sickle cell disease that can benefit everyone who needs it. We have developed an experimental therapy in partnership with UCSF Benioff Children's Hospital and the UCLA Broad Stem Cell Research Center that directly repairs the sickle cell mutation. Briefly, this involves 1) collecting a patient’s blood stem cells, 2) using a brief electrical current to introduce CRISPR-Cas9 enzymes to the extracted stem cells along with a template for correcting the sickle mutation, 3) using chemotherapy to make space in the bone marrow for the edited stem cells, and 4) reintroducing the patient’s own edited cells.
A phase I/II clinical trial that will test this new CRISPR therapy in patients with severe sickle cell disease is being managed by Dr. Mark Walters at UCSF Benioff Children's Hospital in Oakland, California. The trial is currently enrolling patients. Enrollment is being managed by UCSF Benioff Children's Hospital. Learn more >
For background information, learn more about how clinical trials work and more about CRISPR-specific clinical trials. You can find other open trials at clinicaltrials.gov. Clinical trials involve substantial risk and benefits are not guaranteed. Consult with your doctor when deciding if a trial might be right for you.
Driving the Science Forward
The IGI’s interest in sickle cell disease began at the institute’s very beginning. Our first scientific director, Jacob Corn, and his lab developed a novel approach to directly correct the SCD-causing mutation in patient cells, laying the foundational work for the UC Consortium’s genome editing sickle cell trial.
We are working to improve and innovate on new therapies to strive for even better cures that are less risky and burdensome to the patient. This is also crucial to addressing access and affordability: current gene therapies cost millions of dollars and require lengthy hospital stays and specialized facilities not available everywhere. Instead of removing blood stem cells, editing them in the lab, and returning them to the patient, we are developing ways to deliver CRISPR tools directly into the body. Read more about our therapeutic delivery research.
We hope that by continually improving on our sickle cell treatment, we can make it and similar therapies safer and more affordable in the long run.
Delivering Health Justice
 Despite being the first disease ever understood at the molecular level, new drugs and advancements in treatment have lagged behind other, less common genetic diseases. This slow progress is due in part to a long history of discrimination and biased distribution of the risks and benefits of scientific advancements.
Despite being the first disease ever understood at the molecular level, new drugs and advancements in treatment have lagged behind other, less common genetic diseases. This slow progress is due in part to a long history of discrimination and biased distribution of the risks and benefits of scientific advancements.
Over 90% of U.S. patients with SCD are African-American, a demographic that has been historically marginalized and continues to be underserved by the biomedical community. It is important to us that one of the first groups to benefit directly from genome editing technologies is the sickle cell community.
With an opportunity to contribute to health justice, the IGI has built an interdisciplinary initiative to develop a therapy that is curative, affordable, minimally invasive, ethically distributed, and created with guidance from the SCD community.
Guiding principles for the SCD Initiative:
- Ethics: Center a vision of justice and beneficence
- Engagement: Create avenues for input and guidance from the SCD community
- Oversight: Advance best practices for safety and efficacy, with input from the field at large
- Education: Empower the SCD community with resources to understand new therapies
- Access: Ensure that IGI-developed therapies are accessible and affordable. Ours is the only SCD or CRISPR trial run by a non-profit consortium, and we are dedicated to creating innovative IP and commercialization solutions to ensure access.
- Improvement: Continue to work towards creating therapies that are more effective, safer, and have fewer side effects
IGI Team


Melinda Kliegman, Ph.D.
Director, Public Impact

Alex Marson, M.D., Ph.D.
Director, Human Health

Fyodor Urnov, Ph.D.
Director, Technology & Translation

Ross Wilson, Ph.D.
Director, Therapeutic Delivery
Additional Resources
Learn more about the history of sickle cell disease, the progress that has been made with CRISPR therapies, and where the research is heading next:
- Overview: Sickle Cell Disease (National Institutes of Health)
- Patient-focused education:
- IGI Seminar: Responsibly Researching and Communicating About Sickle Cell Disease (Vence Bonham)
- IGI Seminar: A Journey of Pain, Purpose, and Perseverance (Michael Friend)
- Article series: Meet Victoria Gray, the First CRISPR Sickle Cell Patient (NPR)
- Article: CRISPR Clinical Trials: A 2021 Update