Using virus-like particles, researchers find an unexpected explanation for why some coronavirus variants spread faster.
In a new paper published today in the journal Science, researchers at the Innovative Genomics Institute (IGI) at UC Berkeley and Gladstone Institutes used a new method to explore why some variants of SARS-CoV-2, like the Delta variant, are more transmissible and infectious than others.
The new study, a collaboration between the labs of Jennifer Doudna at the IGI and Melanie Ott at Gladstone Institutes, uses virus-like particles instead of live virus, a safer and faster way to explore the effect of different mutations in the virus’s genome. Initial explorations with this method found a surprising result: while most research has focused on mutations in the virus’s spike protein that allows the virus to penetrate human cells, mutations in a different protein, the nucleocapsid protein, appear to be more important for enhancing infectivity.
We spoke with co-first authors Abdullah Syed, Taha Y. Taha, and Takako Tabata to help explain their findings and how this new method could help us create new therapeutic approaches for COVID-19 and other viral diseases:
What is the central question you’re trying to answer? What inspired you to do this project?
Syed: Our big picture question is, why are some variants of SARS-CoV-2 more transmissible or more infectious than others? Does this show us how the virus is adapting to humans? And if there are common ways that the virus adapts to humans, could that be exploited to develop therapeutics?
Variants, like the Delta variant, have small changes in the virus’s genetic code, leading to slightly different versions of key proteins. We were especially interested in looking at whether there were any changes to the genetic code that improved the efficiency of the assembly process for the virus and if that could be affecting infectivity.
What is assembly?
Syed: You can divide up the life cycle of the virus into three parts. The first is entry: how the virus gets in a cell. Then there is replication: where the virus takes over the cell’s machinery to make more copies of the proteins and genetic material that make the virus. The last step is assembly: where the proteins are put together to make a shell and the genetic material is packaged in the middle to make new virus particles to infect other cells.
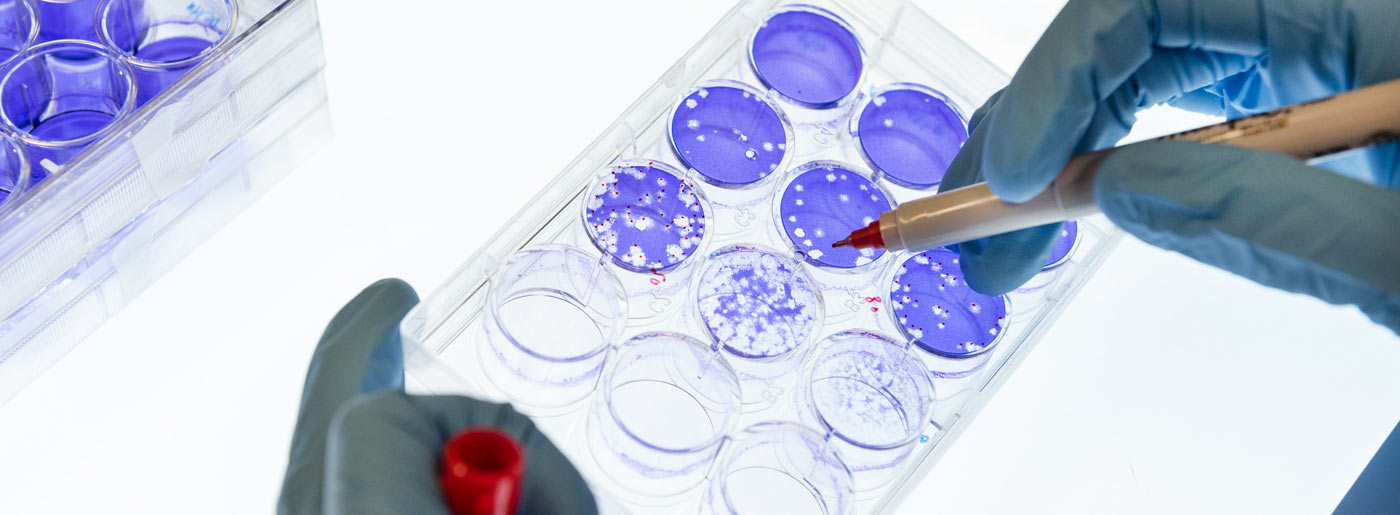
In this paper, you used virus-like particles to study virus replication. What is a virus-like particle? How is it different from a virus?
Taha: Essentially, they have the proteins that make the structure of the virus, but they don’t have the virus’s genetic material inside — they’re hollow.
The cool thing about these virus-like particles is that they do not actually replicate when they infect cells, since they don’t have a genome. So, there is no way for someone to get infected with them. This makes them safe to work with in a lab. We wanted to avoid using the actual SARS-CoV-2 virus as much as possible to keep researchers safe.
Syed: Another advantage is that they are easy to make and modify so we can make many versions of them and use them to test mutations within viral proteins. Making mutant live virus is a long, slow process.
Our key innovation was that we found a sequence in the viral genome that functions as a packaging signal. Meaning, it directs the cell to package the genome inside the protein shell.
The virus genome in this case is made of RNA, not DNA. We found that if we put the packaging signal on a different RNA molecule, that RNA molecule would get packaged into the VLP. This allows us to study the assembly process and compare it in different variants.
What did you find out about the Delta variant using the VLP system?
Tabata: Well, most people are looking at the spike protein that’s on the outside of the virus particle. You’ve probably heard about it in the news. But what we found was that a different protein that people aren’t studying much, the nucleocapsid protein, is key for enhancing infectivity. The Delta variant has changes to the nucleocapsid protein that make it more transmissible. That was very surprising to us.

Why aren’t other researchers looking at the nucleocapsid protein?
Taha: The spike protein is easier to study because it’s on the outside of the virus particle. The nucleocapsid protein is actually inside, so to study it, you either need to work with real viruses — or use VLPs! VLPs are so valuable because you can use them to study any of the virus structural proteins, not just the spike protein.
Syed: You expect there to be mutations in the spike protein, because having a slightly different spike will help it evade the immune response. The nucleocapsid’s job is to package RNA. That should have already been optimized by the virus over millions of years, so it was surprising to find so many mutations in this protein.
Why might a mutation in the nucleocapsid protein be significant?
Syed: When you’re infected by a virus, your cells make a bunch of new virus particles, but most of these are not functional, a very small fraction are complete and contain all of the proper components and are able to infect the next cell. Most viruses have very low efficiency, so a mutation that improves the efficiency of making fully-formed functional particles will enhance transmissibility. That appears to be what these mutations are doing, based on our VLP work.
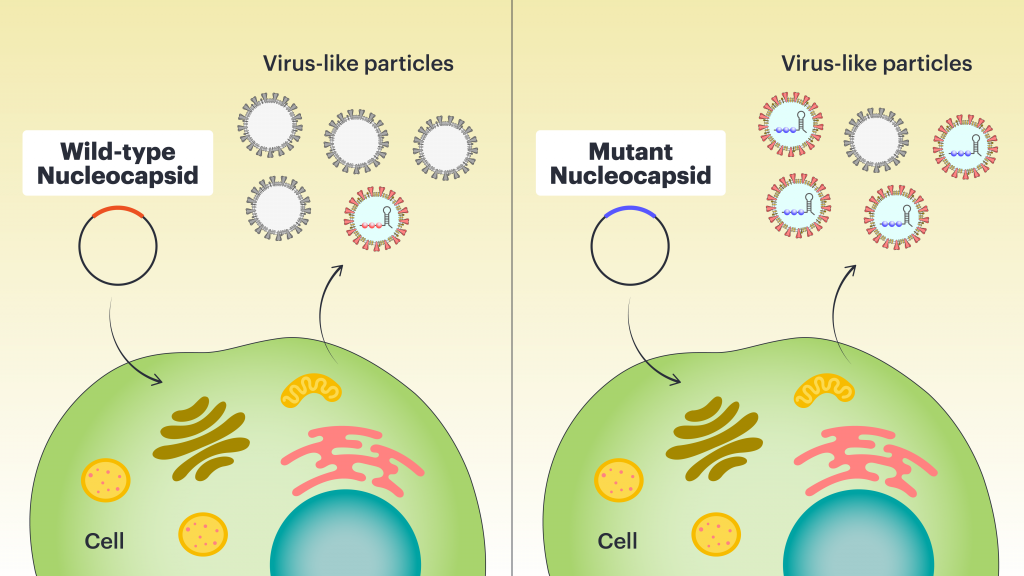
Is there something special about the nucleocapsid protein in the Delta variant?
Syed: One of the mutations found in the nucleocapsid of the Delta variant improves the ability of the nucleocapsid to package RNA by 10 times in VLPs. We found that the total number of particles was the same with or without the mutation but there was more RNA within the VLPs. This matches what has been observed in people infected with the Delta variant in that they produce 10 times more virus in their nose and throat compared to people infected with the older variants.
How can you be sure what you found in VLPs represents what happens with actual viruses?
Tabata: Certain mutations in the nucleocapsid protein made the VLPs assemble better, suggesting that actual SARS-CoV-2 variants with these mutations would assemble better and be more infectious. So to confirm these results, I worked in a highly controlled laboratory setting and tested mutations found in the Delta variant and other SARS-CoV-2 variants in cells. We found that these mutations increased the infectivity and transmissibility of the virus. The virus reproduces faster matching the results we saw with VLPs.
What’s next? Could a similar method be used to study other viruses?
Syed: It would be very useful for other coronaviruses. We know that this family of viruses caused the SARS epidemic in the early 2000s, as well as this current pandemic. So it’s a reasonable assumption that more viruses from this family will jump into humans at some point. But when that happens, we don’t want to grow the entire virus because who knows what these viruses are capable of or how dangerous they are? So we can make a very safe system that can look at them, and even look at coronaviruses that haven’t jumped to humans yet. We can ask, “Can these viruses potentially infect humans?”

Taha: We could also do a lot of work on developing therapies using the VLP system because it’s much faster and safer than using real viruses. You could also test therapeutics that already exist to see whether they actually would work against these different variants, including looking at the efficacy of vaccines against different variants.
Publication: Rapid assessment of SARS-CoV-2 evolved variants using virus-like particles
Learn more about the Innovative Genomics Institute and Gladstone Institutes
Media contact: Andy Murdock