Finding & Fixing Immunodeficiencies with CRISPR
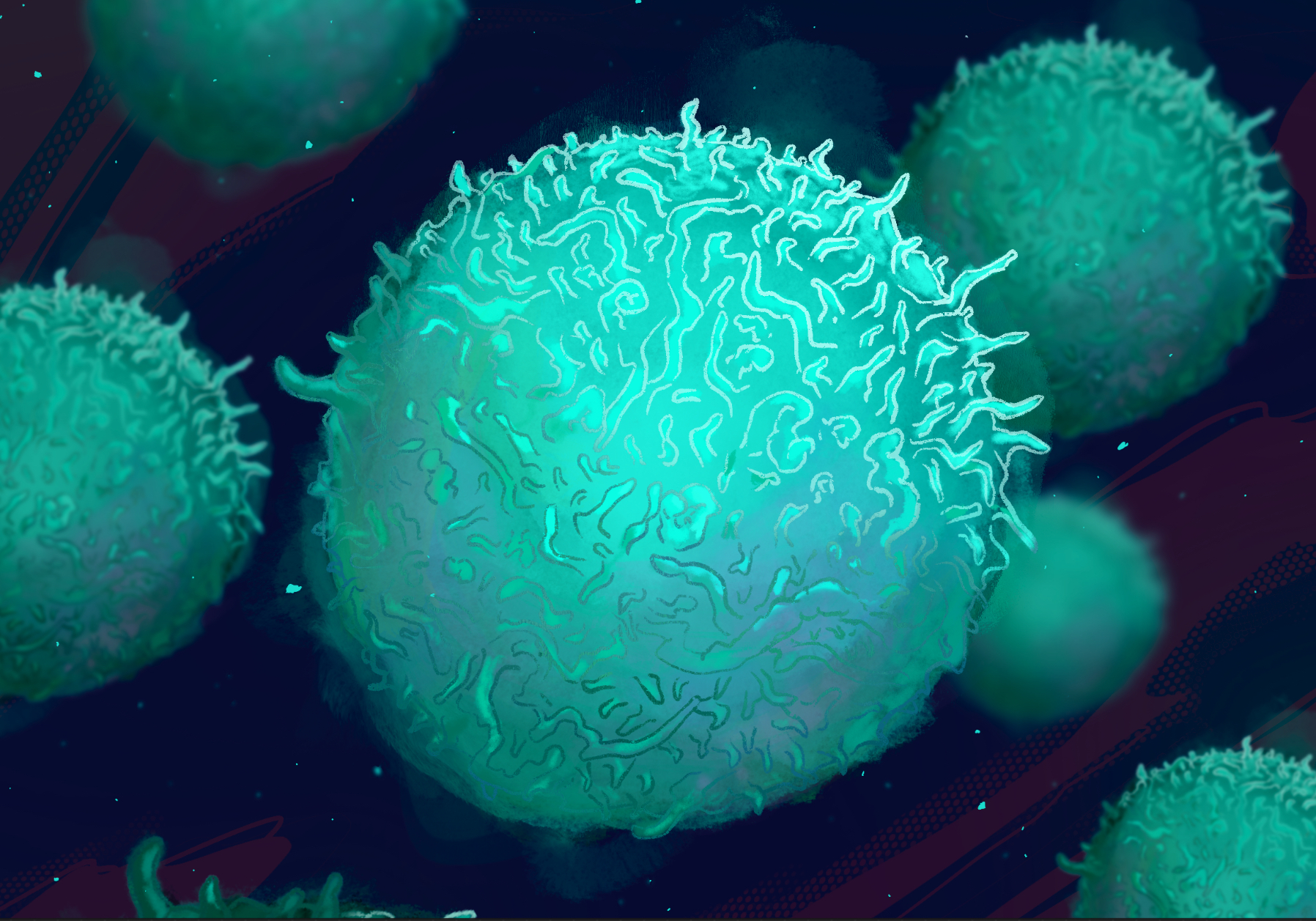
As a physician-scientist, David Nguyen regularly sees patients with immune disorders looking for answers. Sometimes there’s a clear why: a genetic mutation known to cause immunodeficiency. But sometimes sequencing a patient’s DNA turns up unexpected results — unknown mutations in known genes, or mutations in poorly understood genes. In these cases, it’s extremely difficult to diagnose or treat the patient.

“My hope is that my lab becomes the nexus for getting a definitive genetic diagnosis of an immunodeficiency disease and then correcting that mutation using genome editing,” says Nguyen. “The IGI is the right place to do this because we have experts in bringing technology from bench to bedside.”
Nguyen has long been fascinated by immunology and the potential to impact patients’ lives.
“The first successful applications of gene therapy were in immunodeficiencies,” says Nguyen. “Immune cells are easily accessible through the blood for gene editing, so it’s a nice intersection between patient needs and practicality.”
Nguyen completed a Ph.D. in medical engineering at MIT before attending medical school at Stanford. As a graduate student, he focused on using nanoparticles delivery to immune cells. As a medical resident and fellow, he focused on infectious disease, and conducted research in the lab of IGI’s Director of Human Health, Alex Marson, using CRISPR-based tools to edit immune cells.
In his own lab as part of the IGI’s Center for Translational Genomics (CTG), Nguyen is applying this knowledge to create new ways to diagnose and treat genetic immunodeficiencies, also known as primary immunodeficiencies. Utilizing human immune cells left over from blood donations, Nguyen can use CRISPR to recreate a patient’s uncharacterized genetic mutation. Using these cells instead of the more commonly used lab cell lines, like the now-famous HeLa cells, gives more accurate and actionable information.
Using these cells allows me the flexibility to study things in a diversity of genetic backgrounds. On an individual level, we can match a patient’s age, sex, and ethnicity to have the right genetic background to study their mutation and determine if it’s what’s causing their illness or if it might be due to a different mutation or environmental factor. You cannot fix what you don’t know is broken.
Nguyen is also excited about the unique possibilities of using CRISPR versus older gene therapy methods to treat these disorders.
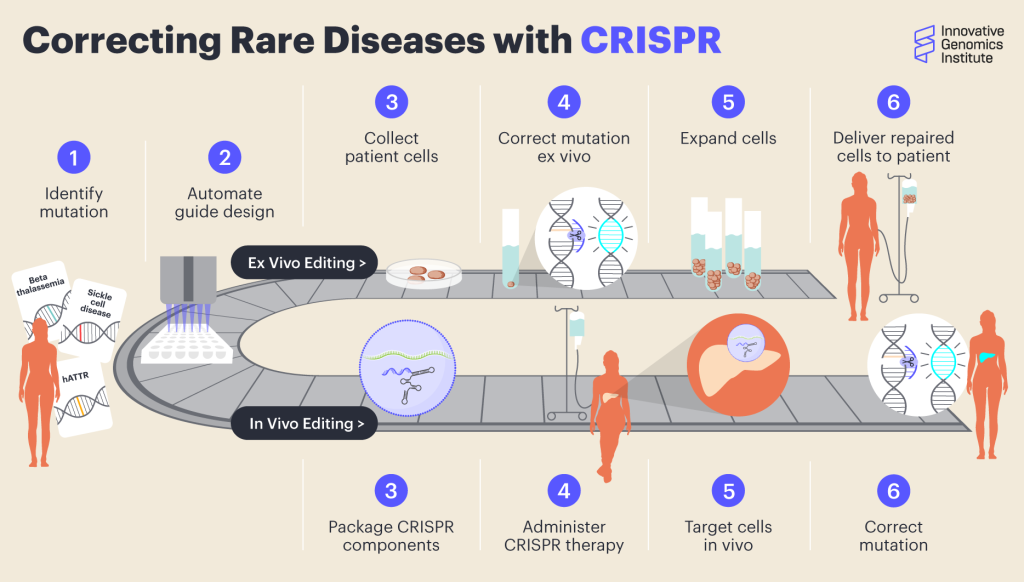
“In classical gene therapy, you use a virus to insert an extra copy of a broken gene. That will work to make a protein, but it’s not well regulated. It only works when constantly making the protein is helpful, but biology is often more complex. The promise of gene-editing therapy is that it can actually fix the problem as opposed to just trying to pave it over,” says Nguyen. “Once you figure out how to do gene editing of one gene in the immune stem cells, it’s not very difficult to do it for any other gene. We’re working on creating CRISPR-based treatments as a platform technology.”
A platform therapy refers to a type of technology where only one part needs to be changed to change to use it for a new application. For CRISPR, this means creating a drug delivery approach where the only thing that would change when using it to treat different mutations is the short, easy-to-make RNA molecule that positions the CRISPR enzymes within the genome.
“Ultimately, we want to deliver a CRISPR cure,” says Nguyen. “And the CTG is a great place to develop this because we have so many different expertises. Fyodor Urnov is an expert in taking something from the lab into a clinical trial. Petros Giannikopoulos is studying editing outcomes and off-target effects. And it’s in close partnership over UCSF, where we have world-experts in cell therapy. Working on the cell therapy aspect would not be possible at most other places in the world. And the funding to do this does not exist at most places.”

The CTG is IGI’s home for translating research to biomedical diagnoses and cures. CTG researchers are united by a focus on creating platforms and other scalable technologies to enable broader access to genomic insights and accelerate therapy development. In addition to addressing genetic immunodeficiencies and autoimmunity, CTG researchers are creating novel therapies for sickle cell disease, cystic fibrosis, and neurologic diseases, as well as clinical assays for rare genetic diseases.
 By
Hope Henderson
By
Hope Henderson