Prioritizing Sickle Cell Patients: A Chance to Mend Broken Ties
I’ve lived with sickle cell disease for 34 years now. Never have I imagined that a cure would be imminent, at least not within my lifetime. In fact, I remember days as an adolescent when my pediatric hematologist would tell me I’d be lucky to live long enough to experience college.

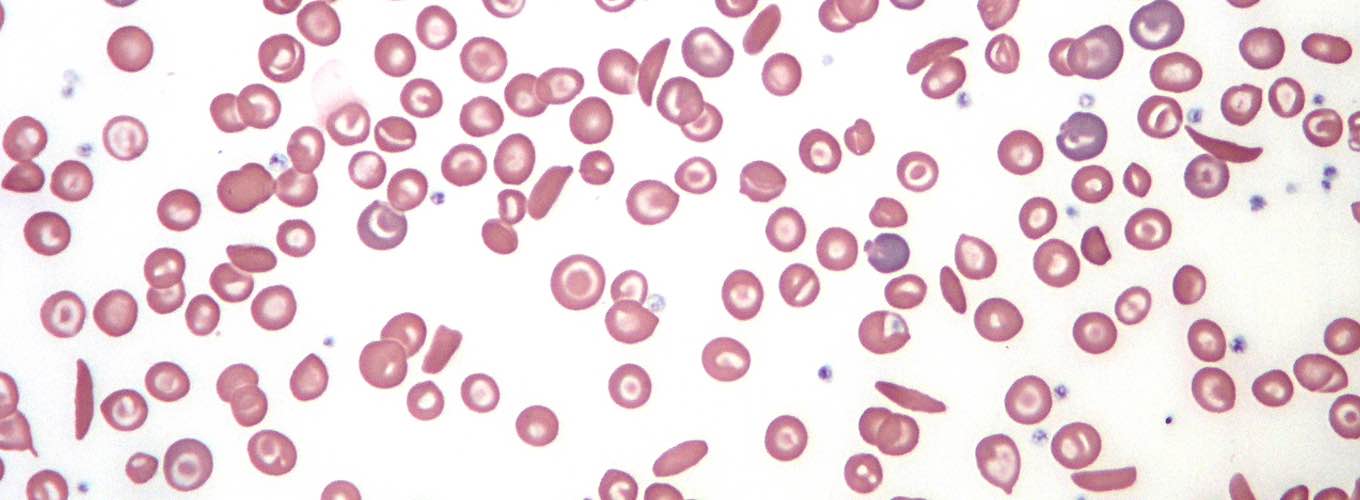
It’s an everyday struggle living with an illness that penetrates all areas of my body where blood flows. Unlike most children who live with sickle cell disease (SCD), my daily struggle didn’t include constant visits to the emergency room plagued by excruciating pain (although I’d experience a great deal of pain in adulthood). Instead, the pain came from my monthly blood transfusions, which became a routine therapy after a stroke, that ultimately devastated my veins. Not long after came the nightly subcutaneously-administered iron chelation therapy overnight infusions. This nightly treatment led my teachers to question whether I was being abused at home (which by the way wasn’t the case at all- I come from a loving household, thank you) due to the common occurrence of bruising and occasional swelling on my arms & legs.
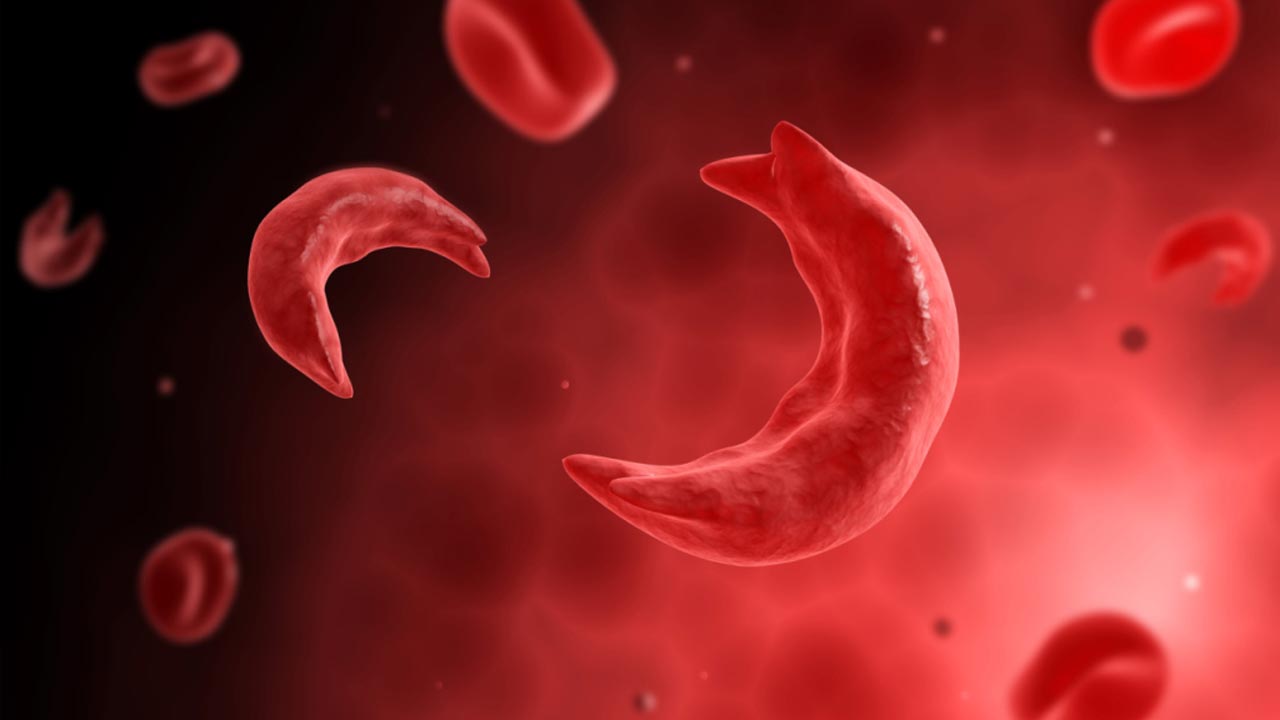
Fast forward 30 years and I’m still receiving the same exact method of treatment. I have continued my tri-weekly exchange transfusion therapy, sacrificing my veins for over a decade after several Port-A-Caths have failed me. It’s extremely disheartening that such a devastating disease, one that’s well studied and even historically credited as the first biomolecular illness (Pauling, 1951), has only gained one FDA-approved drug within the last 20 years. This sole drug, Endari (aka L-Glutamine), doesn’t even target the root cause of the half-moon-shaped red blood cells.
Why has there been no progress to treat such a horrific disease? Is there truly no scientific incentive? We cannot ignore the fact that sickle cell disease predominantly affects African Americans (about 90% of cases) as compared to cystic fibrosis, which mostly affects Caucasian Americans and was originally identified nearly three decades after SCD. We cannot ignore the history of African Americans being mistreated by the biomedical research community; e.g. Henrietta Lacks and the Tuskegee syphilis experimentees. It’s hard not to consider the thought of a purposeful neglect of the sickle cell disease community.
As feelings of biomedical distrust continue to course through minority communities, particularly amongst African Americans, recent reports of CRISPR-Cas9 genome editing technology may offer a small step towards mending a shattered relationship. Some researchers leading the development of this technology have set their initial focus on sickle cell disease, offering a chance to correct historic mistreatment. Scientists will attempt to use CRISPR to target the root cause of SCD, a single mutation in the entire human genome.
As cofounder of the Minority Coalition for Precision Medicine (MCPM), I’ve come to personally know many incredible scientists directly involved with the development of CRISPR-Cas9 to treat SCD. One of them is Dr. George Church. Genuine interaction and instruction from Dr. Church have played a major role in my personal strengthening of trust towards the scientific community. Through our combined efforts in working with the Personal Genetics Education Program (pgEd) at Harvard Medical School, we have fostered conversations on personal genetics and precision medicine. Open dialogue focused on the past, present, and future of genetics has allowed us to educate cohorts within minority communities throughout the US. As a patient and as a person of faith, I’ve seen the impact of these conversations firsthand. Often, pairing faith-based leaders with acclaimed scientific researchers can improve the impact and acceptance of emerging genetic technologies throughout diverse minority communities.
Our work has only just begun. The Minority Coalition for Precision Medicine will continue the conversation in mid-February 2018, in Berkeley, California with the FREEDOM with CRISPR Conference. Caribou Biosciences, a biotechnology company developing CRISPR-Cas9 for human therapeutics, along with MCPM, is hosting a workshop around the topic of sickle cell disease and other potential applications for genome editing. I encourage others to join in on this conversation. Any interested faith-based and/or community leaders should take this opportunity to rebuild trust between the biomedical and minority communities.
Visit our website for more information on how you can get involved.
 By
Shakir Cannon
By
Shakir Cannon