A $1.25 million gift will support engineering lipid nanoparticles for brain delivery
A new project co-led by IGI founder Jennifer Doudna and Doudna lab researcher Kai Chen has been awarded $1.25 million from the Rett Syndrome Research Trust (RSRT) to develop CRISPR tools to edit the brain. The ultimate aim of this research is to create CRISPR-based therapies for Rett syndrome, a severe neurodevelopmental disorder.

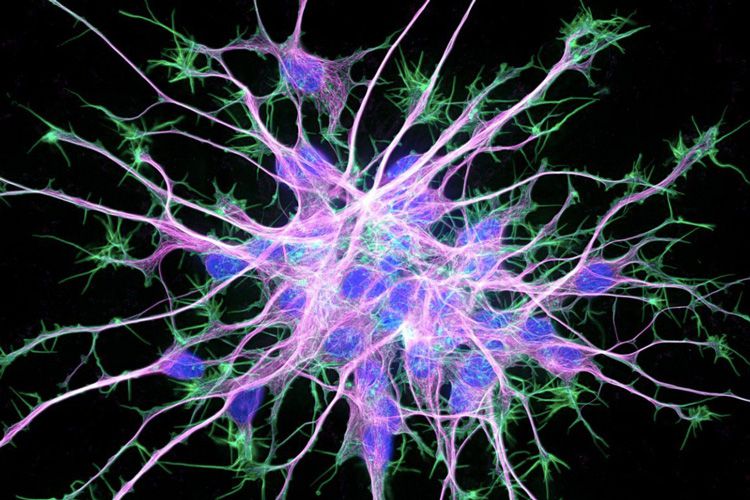
RSRT became interested in supporting IGI research following a 2024 publication in Nature Communications on advances to genome editing in the mouse brain. In the paper, first author Chen and Doudna lab collaborators used small cell-penetrating peptides, which are like miniature protein fragments, to deliver a Cas9 ribonucleoprotein without packaging it into a bulkier delivery system like a virus.
With the new funding, the Doudna lab will collaborate with IGI Investigator Niren Murthy, whose research focuses on developing new ways to deliver drugs and genomic therapies. Together, they are focused on developing lipid nanoparticles (LNPs) for delivery to the brain.
“LNPs are a great delivery method since they provoke very little immune response, and could even be used multiple times in the same patient if necessary, unlike virally delivered therapies,” says Chen.
At least two CRISPR-based therapies using LNPs to deliver drugs to the liver are currently in clinical trials and showing very encouraging early results.
Delivering CRISPR to specific tissues and cells is one of the biggest challenges in the field and the brain is one of the most challenging organs for delivery. One factor is that the brain is protected by a membrane known as the blood-brain barrier. The blood-brain barrier acts as a filter, keeping harmful substances and pathogens from penetrating the brain. But it also keeps CRISPR-based molecules from traveling from the blood to the brain, so systemic administration (e.g., through an IV) is not effective for brain delivery of gene-editing treatments.
Research on animal models of brain disorders sometimes uses direct injection of therapeutic molecules into a relevant brain area. This was safely done in human patients in 2022 in a small clinical trial of gene therapy for a different neurodevelopmental disorder, Tay-Sachs disease. While some brain disorders like Parkinson’s disease affect only a particular small region of the brain, others including Rett syndrome and Alzheimer’s disease affect the brain more globally. For these conditions, an effective treatment would need to spread throughout the brain tissue, not just remain in the small region where it was injected.
“Our main challenge in this project is how you can get the editing material to diffuse across the entire brain,” says Chen.
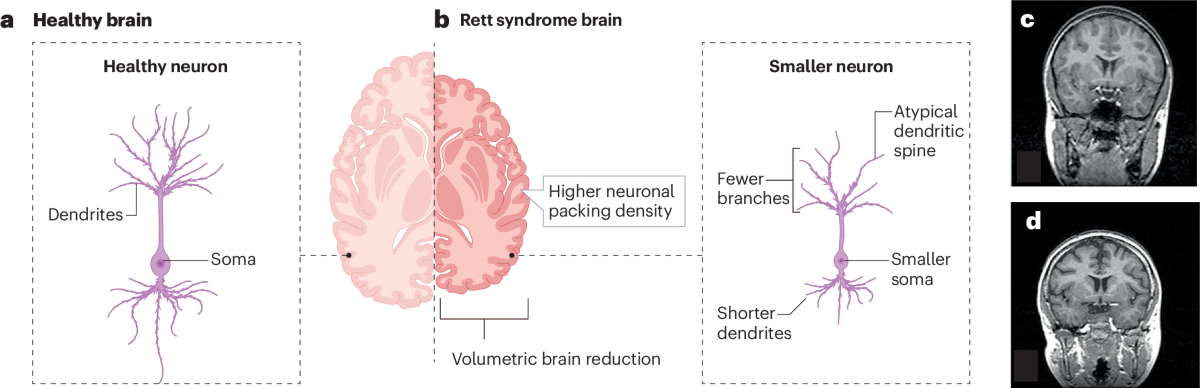
The funding partner, RSRT, is a nonprofit organization that funds research aimed at creating genomic treatments for Rett syndrome. Rett syndrome is a genetic disorder affecting approximately one in every 10,000 girls and women. It is caused by mutations to the MECP2 gene on the X chromosome that reduce the function and/or quantity of the MECP2 protein in the brain. Girls with Rett syndrome undergo a dramatic developmental regression in early childhood, leading to total loss of speech, loss of motor control, digestive and respiratory problems, and more. There is currently one FDA-approved treatment for Rett syndrome, but many patients cannot tolerate the medication and less than half of those that can show improvement.
“We are excited to partner with RSRT on this new project, which taps into one of IGI’s core missions: advancing innovative technologies to treat rare diseases,” says Doudna. “Enabling brain delivery will not only be crucial for treating Rett syndrome, a devastating condition that almost exclusively affects girls and women, but for a wide-range of brain disorders and diseases.”
Ultimately, Doudna and Chen hope to create treatments for Rett syndrome using base editing, a form of CRISPR-based genome-editing that can be used to make small changes to DNA, as well as developing ways to use CRISPR to add, or “knock-in,” healthy versions of the MECP2 gene.
Disclosure: Hope Henderson occasionally writes for the Rett Syndrome Research Trust, the funder of this project.